Research in lung health
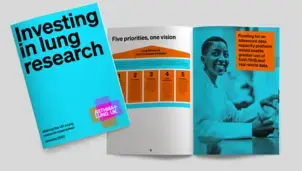
Lung Research Grand Challenges
Our research and applying for funding
Research influencing
How we're pushing for better research into lung conditions
Blog
Visit the research section of our blog for news and stories about our work in respiratory
Research
Join the fight!
Stay informed about the work we do, the latest advice, support, research and campaigning news, as well as ways you can support our work by signing up to our regular newsletter.