About COPD
Find out what COPD is, what the symptoms are, and how it’s diagnosed and treated. We also have information on managing and treating COPD flare-ups (exacerbations).

What is Chronic Obstructive Pulmonary Disease (COPD)?
Chronic obstructive pulmonary disease (COPD) is a group of lung conditions affecting your breathing.
How is COPD diagnosed?
If your doctor thinks you might have COPD, your doctor will ask you some questions and suggest some breathing tests.

What are the treatments for COPD?
Your healthcare professional can prescribe treatments to improve symptoms and to help prevent a flare-up.

Medications for COPD
Your doctor will decide with you which medications to use depending on how severe your COPD is, how it affects your everyday life, and any side effects you may have had.
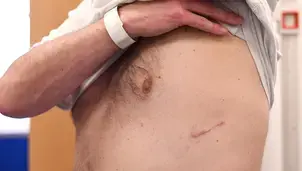
Lung volume reduction procedures
Find out what lung volume reduction procedures are and who can benefit from them.

What can you do to manage your COPD?
Managing your condition can help you to feel better and take some control of your life.

Managing COPD flare-ups
A flare-up – sometimes called an exacerbation – is when your symptoms become particularly severe.

Your COPD self-management plan
Self-management of your COPD will help give you control of your condition. On this page, we explain why COPD self-management is important and provide links for you to download your own COPD self-management plan.
Severe COPD
Some people with COPD have mild lung damage and few symptoms. Others have very damaged lungs and can be especially limited by breathlessness – these people would be considered to have a severe case of COPD.

Chronic bronchitis
Along with emphysema, chronic bronchitis is one of the main conditions of chronic obstructive pulmonary disease (COPD).

Emphysema
Emphysema is a type of lung damage that can happen with COPD. On this page find out more about emphysema.
COPD resources
Resources to help you self-manage your COPD.

COPD Patient Passport
Find out if you're getting the best care for your COPD.

COPD self-management plan
Download a COPD self-management plan.

First steps to living with COPD
Find out what to do if you've just been diagnosed.




