What is lung volume reduction (LVR)?
Lung volume reduction (LVR) is a treatment for emphysema. Emphysema is a type of COPD (chronic obstructive pulmonary disease). LVR is a procedure that removes the most damaged parts of your lungs so that the healthier parts can work better. The treatment should make it easier for you to breathe.
LVR may be done using:
- Lung volume reduction surgery (LVRS). A surgeon will operate and remove the most damaged parts of your lung.
- Endobronchial valves (EBV), or bronchoscopic lung volume reduction (BLVR). Valves are placed into your airways to stop air from getting to the most damaged parts of your lung. This causes these parts to shrink and make more space for the healthier parts of your lung to work.
- Experimental treatments. Your specialist can talk about these options with you.
What are the benefits of LVR?
LVR can improve:
- how well your lungs work
- breathlessness
- your ability to do daily activities
- your quality of life
- your life expectancy.
Who can have lung volume reduction (LVR)?
Lung volume reduction (LVR) can be very effective, but only around 1 to 2 in 100 people with emphysema are likely to be suitable.
LVR is available on the NHS in England. It should be available to anybody with severe emphysema who will benefit from it. If you live in Scotland, Wales or Northern Ireland and think LVR might work for you, you should talk to your GP or specialist.
Pulmonary rehabilitation (PR) is an effective treatment for breathlessness. You have to complete a course of PR before you can have LVR. Your PR team will be able to talk to you about LVR and whether you may be suitable.
If you’re still limited by breathlessness after a course of PR, your healthcare professional should consider whether you may be suitable for a lung volume reduction procedure.
Your lung specialist will review whether LVR may be right for you if:
- you have severe emphysema
- you are limited by breathlessness, meaning you get breathless after walking for a few minutes on flat ground
- you have not smoked in at least four months
- you have completed pulmonary rehabilitation (PR) within the last 12 months or are taking part in a post-PR exercise programme
- you are not too underweight or frail
- you do not have other long-term conditions that mean that LVR might not be safe or effective for you, like pulmonary fibrosis or heart failure
- your lung function tests show that you are someone who is likely to benefit. This usually means that the amount of air you can blow out in one second is less than half of what it should be. The amount of air that stays trapped in your lungs when you breathe out also needs to be higher than normal for you to have LVR.
If these apply to you, your specialist should refer you to a multidisciplinary team (MDT) to be assessed.
The MDT will include different lung specialists including doctors, a surgeon and a specialist nurse. They will assess you and decide:
- whether lung volume reduction is right for you
- if so, what type or types of lung volume reduction might be best for you.
Why would lung volume reduction (LVR) not be right for me?
Lung volume reduction might not work for you if:
- you have other long-term conditions as well as emphysema, like pulmonary fibrosis, severe pulmonary hypertension, or heart failure
- your emphysema is evenly spread across your lungs. This makes finding suitable parts of your lung to target harder.
If LVR is not right for you, your specialist can speak to you about other treatment options.
What tests will I need?
You’ll need to have tests to make sure lung volume reduction (LVR) is right for you.
The tests can include:
- A CT scan. This will find out if your emphysema is evenly spread (homogeneous) or uneven and patchy (heterogeneous). If it is uneven, lung volume reduction is more likely to work because there are areas that can be removed or blocked off. A CT scan can also detect other problems like fibrosis or bronchiectasis that might mean LVR is not possible.
- A spirometry test. This measures how much air you can blow out in one second.
- A gas transfer test. This measures how well oxygen passes from your lungs to your blood.
- A lung volume test. This measures how much air is left in your lungs after you breathe out.
- A walk test to measure your ability to exercise and overall fitness.
- A lung ventilation perfusion scan (sometimes called a VQ scan). This scan works by injecting you with a special material that shows areas of your lungs that don’t have much blood supply. These areas don’t help your breathing, so they may be able to be removed.
- An echocardiogram to see how well your heart is working.
Lung volume reduction surgery
Lung volume reduction surgery is an operation which removes the most damaged parts of your lung so the healthier parts of your lung can work better. This should make your breathing more comfortable.
Lung volume reduction surgery is usually a keyhole surgery. Your surgeon will use a special tool to cut away and staple your lung shut at the same time. This will seal it and prevent or reduce any air leaks.
The procedure is done using general anaesthetic, so you are asleep when it happens. It takes around 1 to 2 hours.
What is keyhole surgery?
Keyhole surgery is a type of surgery that uses small cuts and a camera put inside your chest. It takes less time to recover from keyhole surgery than other types of surgery where larger cuts are made.

Recovery
How long you spend in hospital afterwards varies from person to person, but it is usually 4 to 10 days. After the procedure you will have one or more chest drains put in place to allow air to escape until the lung heals.
For around 1 to 3 months after the surgery, you may experience some extra coughing, pain and breathlessness, but most people find they can breathe more easily.
Endobronchial valves (EBV)
Endobronchial valves (EBV) are another form of lung volume reduction. They are small, one-way valves placed in your lungs to block off the most damaged part of the lung. This is done using a small flexible camera (a bronchoscope).
The valves allow air to leave the damaged area of the lung, but no air can get in so this area shrinks down to almost nothing. Like lung volume reduction surgery, this means the lungs do not inflate more than they should and makes room for healthier parts of the lung to move.
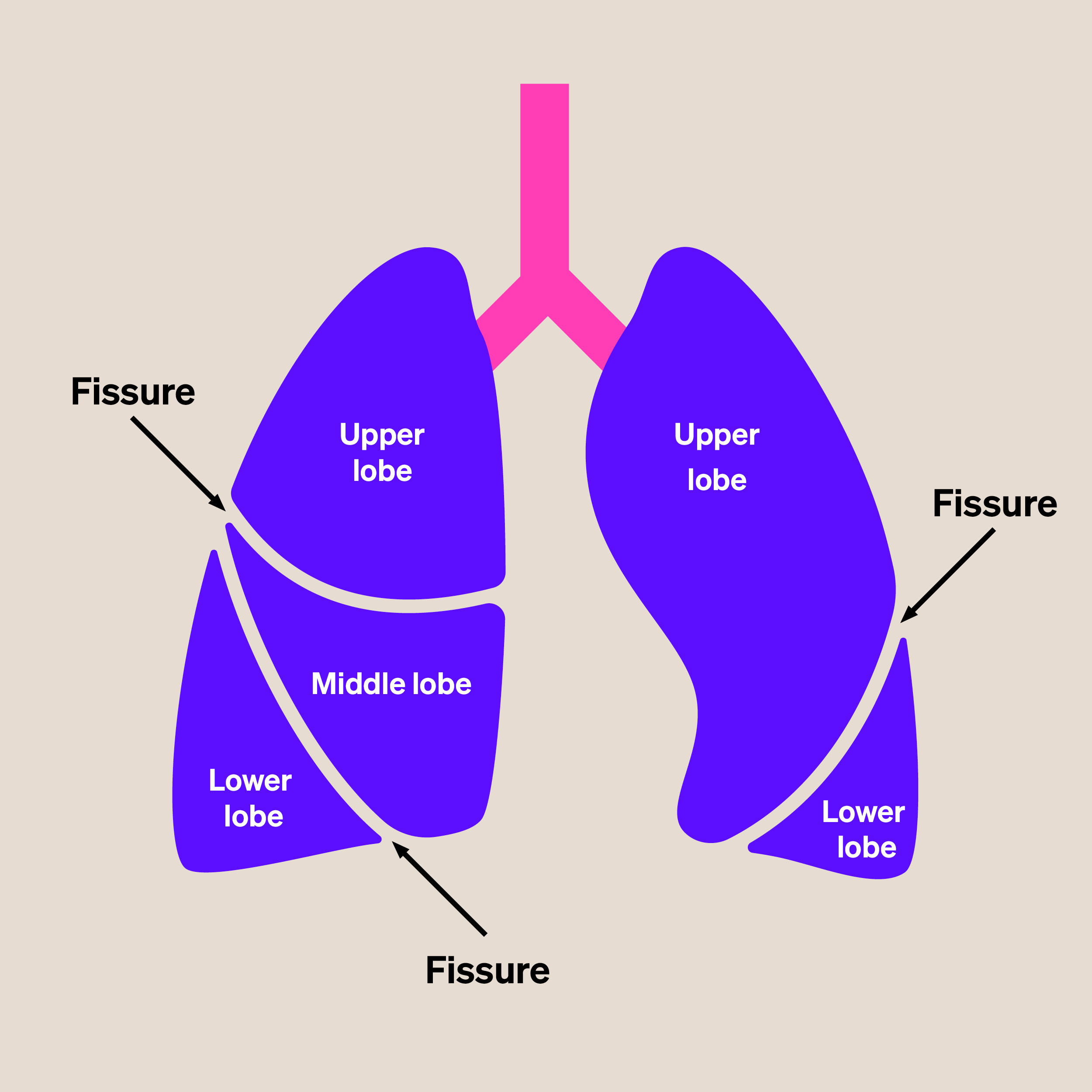
EBV only works if it is possible to treat a whole lobe of the lung. If your emphysema has broken down the division (fissure) between the lobes of your lung, then the procedure will not work. This is because even though the airways are blocked by the valves, air can still get into the lungs another way. When this happens, it is called collateral ventilation. This can be measured using a procedure called Chartis, which uses a catheter with a balloon at the tip. If you have collateral ventilation, EBV will not work for you.
EBVs are usually put in under general anaesthetic so that you are asleep during the procedure. Putting the valves in takes less than an hour.
This procedure is sometimes called bronchoscopic lung volume reduction (BLVR).
Recovery
You’ll need to stay in hospital for 2 to 3 nights after the procedure. Once you’re home you should recover after 2 to 3 weeks.
The most common risk of lung volume reduction is an air leak. This can cause your lung to collapse (a pneumothorax). This happens to around 1 in 4 people who undergo EBV. It normally happens in the first few days after the procedure, when you’re still in hospital. This means it can be treated easily. An air leak may heal by itself. If not, you will need to have a chest drain inserted until your lung recovers.
Your multidisciplinary team (MDT) should talk to you about the risks with you before your treatment.
Are valves or surgery better?
In patients who are eligible, both lung volume reduction surgery (LVRS) and endobronchial valves (EBV) can improve your lung function, ability to exercise, quality of life and life expectancy. Recent studies have shown that both procedures are equally safe and effective.
The right approach depends on the pattern of emphysema, which your MDT will be able to see in your CT scan. Sometimes only EBV or only lung volume reduction surgery is an option. Sometimes either treatment might be effective. Your MDT will discuss with you which procedure is right for you.
Experimental techniques
Clinical trials are developing new experimental techniques for lung volume reduction.
These include:
- using steam to make the areas of the lung that are not working properly scar over, so they shrink
- targeting the nerves in the lung to improve airway relaxation.
These techniques are being evaluated in specialist centres. They are currently only available as part of clinical trials. If you are interested in them, talk to your GP or specialist.
Lung volume reduction webinars
Professor Nick Hopkinson, Asthma + Lung UK’s Medical Director, has produced two webinars to explain what lung volume reduction procedures involve:
- Watch the webinar for patients. This is an introduction to lung volume reduction. It is useful if you have emphysema or are currently doing pulmonary rehabilitation.
- Watch the webinar for healthcare professionals. This is an introduction to lung volume reduction aimed at healthcare professionals. It is useful if you are a physiotherapist or a healthcare professional involved in pulmonary rehabilitation. It can help you discuss lung volume reduction surgery or endobronchial valves with patients and increase your understanding of who to recommend for lung volume reduction.




