If I have Long COVID, am I still infectious?
No. People are infectious for up to 10 days after developing COVID-19 symptoms. People are not infectious after this point.
What is Long COVID?
Long COVID is used to describe symptoms that last for four weeks or more after having a confirmed or suspected case of COVID-19.
Long COVID does not seem to be linked with how ill you were when you had COVID-19.
Long COVID symptoms
If you have had coronavirus, you may find that you have continuing symptoms that last for weeks or months after the initial infection.
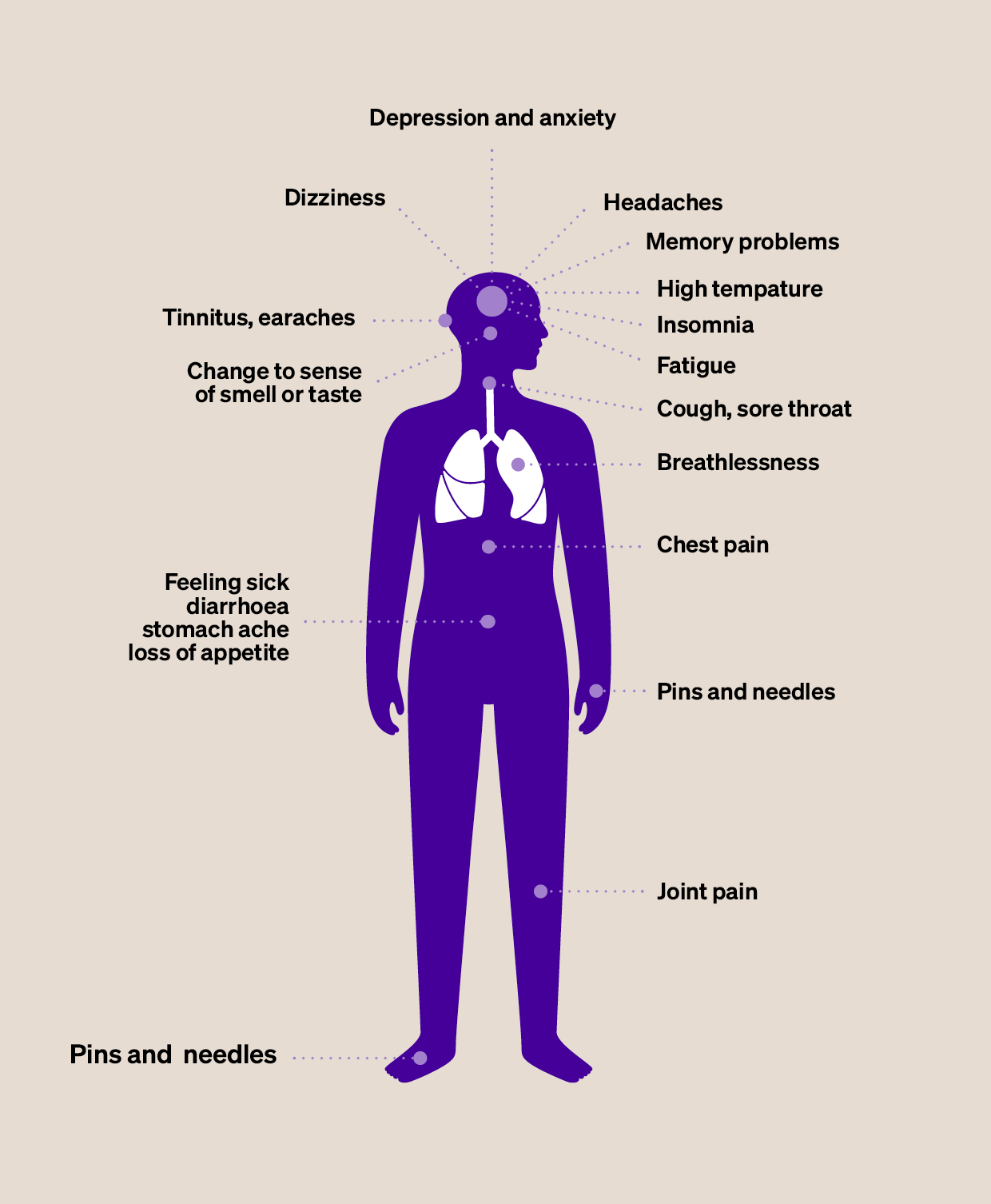
Long COVID can affect any part of the body and you may have lots of different symptoms. Your symptoms may change or come and go over time.
You might have some, or all, of these symptoms:
- breathlessness
- extreme tiredness (fatigue)
- problems with memory and concentration (known as ‘brain fog’)
- a cough that’s been ongoing since you’ve had COVID-19
- chest pain or tightness
- difficulty sleeping
- dizziness
- joint pain
- heart palpitations (a more noticeable heartbeat)
- depression and anxiety
- a ringing sound in your ears or earaches
- feeling sick, diarrhoea, stomach aches, or loss of appetite
- a high temperature, cough, headaches, sore throat, or changes to your sense of smell or taste
- pins and needles
- rashes.
Understanding your symptoms
If you’re living with longer-term symptoms of COVID-19, you might need more help and support than you’re currently getting.
Fill out the My Long COVID Needs assessment to help you understand your needs and get advice on what you should do next.
You can use your assessment results to help you explain your symptoms to your GP. Showing your summary report to your GP may make it easier to get referred to local support services, such as a Long COVID Clinic, or help for problems such as work, money, and mental wellbeing.
When to get help
If you're worried about symptoms four weeks or more after having COVID-19, contact your GP. They will ask about your symptoms and the impact they are having on your life. They will also try to find out if there are any other possible causes for your symptoms.
These could potentially be serious, so it’s important that you get help as soon as possible.
If you have another medical condition and it’s been getting worse since you’ve had COVID-19, speak to your GP.
Treatment and support
Your GP will talk to you about the care and support you might need. This might include advice on how to manage your symptoms at home.
If your symptoms affect your day-to-day life, your GP may refer you to specific Long COVID services or a specialist that can help with your specific symptoms. This could be a physiotherapist, a dietitian, an occupational therapist, or another health care professional.
We have more information and support on managing breathlessness, a cough, and your energy levels. We also have support for your mental wellbeing.
We also have advice on the care you can expect for Long Covid from the NHS.
If you have been unable to work, you may need help with the cost of living. We have lots of information about different benefits you may be entitled to, including help with heating and food costs.
Online support
Your GP may refer you to online support, such as the NHS Your COVID Recovery programme. This is an online rehabilitation app designed to support your physical and emotional recovery if you have ongoing COVID-19 symptoms.
Find out more on the Your COVID Recovery website.
When will I get back to normal?
Recovery is different for everyone. You might find you make a full recovery within 12 weeks of getting coronavirus, but you might find that your symptoms last a lot longer. Some people also find that their symptoms feel better on some days and worse on others.
What to think about during your recovery
- Allow yourself time. It’s important not to expect too much from yourself as you recover.
- Rest when you need to. Doing too much too soon could make your recovery longer. You can also try relaxation techniques to help your body reduce physical tension. Mind has more information on relaxation exercises.
- Set yourself small targets. Once your energy levels have improved, you can plan to do more if you feel up to it.
- Get your COVID-19 vaccines and booster if you haven’t already. You can read more about the COVID-19 vaccine, including answers to some common questions, on our vaccine FAQ.




